Procedures performed under Sedation and Fluoroscopy
Radio waves heat nerve endings and decrease transmission of pain signals to the brain.
Sacroillac Joint Injections
This is done by numbing the sacroiliac joint with local anesthetic (e.g. lidocaine).
These injections are given directly into the muscle.
Spinal Cord Stimulation (Trial)
Before implanting a permanent Spinal Cord Stimulator, a
temporary device is placed to assess effectiveness of this therapy.
Commonly injected joints include the knee, shoulder,
ankle, elbow, wrist, base of the thumb, and small joints of the hands and feet
Facet joints are small joints located in pairs on the back of the
spine that provide stability to the spine and allow the spine to move and be flexible.
Occipital nerve blocks refers to injections performed at the top of the neck where it meets up with the skull.
Massage is known to affect the circulation of blood, reduce muscular tension and enhance tissue healing.
Transforaminal Epidural Injections
This procedure will deliver a medication formulation to more specifically address pain in the back and down the leg.
Caudal Epidural Injections
A caudal steroid injection can help reduce pain causing inflammation in as little as one or two injections.
Cervical Epidural Injections
Cervical or Neck epidural steroid injections are frequently used treatment for chronic neck and arm pain syndromes.
This is the most sophisticated form of electrotherapy available,
combining all known forms of electromedical therapy, in addition to this revolutionary therapy.
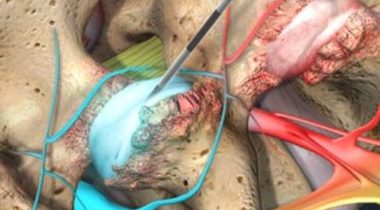
Radiofrequency Ablation (RFA)
RFA uses radio waves to heat nerve endings, disrupting their ability to send pain signals to the brain. This treatment is effective for chronic pain in the neck, back, or joints—especially in the spine and hips.
The procedure begins with diagnostic injections to identify the correct nerves. Using fluoroscopic (X-ray) guidance, a small needle delivers heat directly to the targeted nerve area. Local anesthesia and light sedation are typically used for comfort.
RFA is minimally invasive, and many patients experience significant pain relief lasting 6 to 12 months. Full results usually appear within 2 to 3 weeks after the nerves are fully deactivated.
RFA may be referred to as medial branch neurotomy, rhizotomy, or radiofrequency neurotomy.
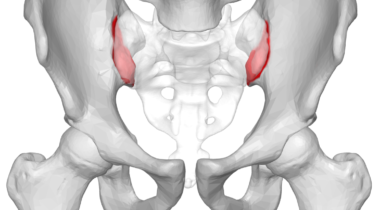
Sacroiliac Joint Injections (SJI)
This injection targets inflammation and pain in the sacroiliac (SI) joint—where the spine meets the pelvis. A combination of local anesthetic and corticosteroid is used to reduce swelling and block pain signals from the joint.
SJI is recommended for patients experiencing pain in the lower back, buttocks, groin, or legs caused by arthritis or SI joint dysfunction. Pain relief may last several months, often up to 10 months for some patients.
The procedure is performed in-office using live X-ray guidance (fluoroscopy) for precision. After numbing the area, the doctor injects the medication directly into or near the joint. IV sedation is available for comfort during the procedure.
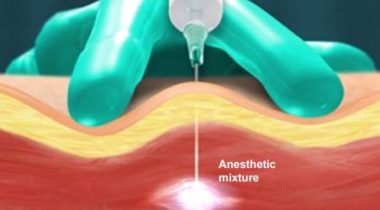
Trigger Point Injections (TPI)
TPI is a quick, outpatient procedure designed to relieve muscle pain caused by trigger points—small, tender knots in muscle or fascia. These knots may cause localized or referred pain and are commonly treated with a mix of local anesthetic and steroid.
TPIs are effective for patients with neck or back pain, tension headaches, or Myofascial Pain Syndrome. The treatment can provide rapid relief and restore mobility to affected areas.
During the procedure, the doctor identifies the trigger point by feel and inserts a fine needle to deliver the injection. This helps inactivate the trigger point and relieve pain, often within minutes.
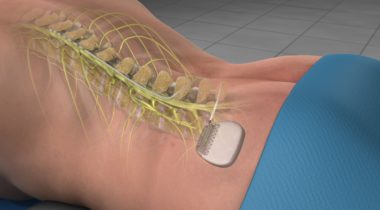
Spinal Cord Stimulator
A spinal cord stimulator (SCS) is a small device that delivers pulsed electrical signals to the spinal cord to reduce chronic pain. It works similarly to a pacemaker, intercepting pain signals before they reach the brain. This can result in substantial relief and reduce the need for pain medications.
The SCS system is implanted in the body and includes a pulse generator and thin wires (leads) that are placed near the spinal cord. Once activated, it sends mild electrical pulses to the nerves, modifying how pain is experienced.
This treatment is typically recommended for patients with chronic back, leg, or arm pain that hasn’t responded well to other therapies. A trial period is usually performed first to ensure the device provides significant pain relief before permanent implantation.
Joint Injections
Joint injections are a targeted method of delivering medications directly into affected joints to relieve pain, reduce inflammation, and restore mobility. As we age, the balance between cartilage production and loss shifts, often leading to arthritis-related joint pain.
At Sebring Pain Management and Rehabilitation Center, Dr. Reid performs joint injections using fluoroscopy (live X-ray) to ensure precise needle placement. Sedation options are available for your comfort, and procedures are often done in-office with minimal recovery time.
Who needs this procedure?
Patients with osteoarthritis or other degenerative joint conditions who are limited in their daily activities due to joint pain may benefit. Common sites for injections include the knees, shoulders, and hips.
How effective are Joint Injections?
Many patients experience pain relief lasting from several months to over a year. Injections may also reduce swelling and improve joint function by limiting further inflammatory activity.
Facet Joint Injections
Facet joint injections are targeted treatments used to relieve pain caused by inflammation in the small joints along the spine. These joints support movement like twisting and bending, and when affected by arthritis or injury, can become a major source of discomfort.
Using fluoroscopic guidance, Dr. Reid injects a mix of anesthetic and steroid into the affected joints to both reduce pain and identify the pain source.
Who needs this procedure?
Pain caused by facet joints can appear in the back, buttocks, neck, or limbs. Dr. Reid can help determine if your symptoms align with this type of joint issue.
How effective are Facet Joint Injections?
Relief is often felt immediately due to the anesthetic, with steroid effects lasting weeks to months. Injections can be repeated as needed.
Occipital Nerve Block
The occipital nerves at the base of the skull can become irritated, leading to chronic headaches and neck pain. When inflamed, they often contribute to migraines and cervicogenic headaches.
This quick outpatient injection, typically performed by Dr. Reid, uses a local anesthetic—sometimes with a steroid—to calm the nerves and reduce pain signals.
Who needs this procedure?
If you experience pain starting at the base of your skull that radiates upward, especially with migraines or cluster headaches, this treatment may be right for you.
How effective is it?
Occipital nerve blocks have shown to provide relief lasting several months, especially in patients with cervicogenic headaches.
Massage Therapy
At Sebring Pain Management and Rehabilitation Center, our certified massage therapist uses targeted techniques to treat muscles, tendons, ligaments, and connective tissue, improving both physical and mental wellness.
Massage boosts circulation, supports the lymphatic system, helps regulate hormones, and reduces pain. It’s especially helpful for chronic low-back pain, muscle stiffness, and recovery from injury.
What are some benefits?
Massage improves mobility, reduces tension, and accelerates recovery. It’s effective for fibromyalgia, fatigue, and stress-related discomfort. Swedish massage is commonly used for relief and relaxation.
Schedule your massage with us today.
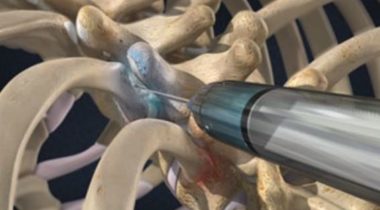
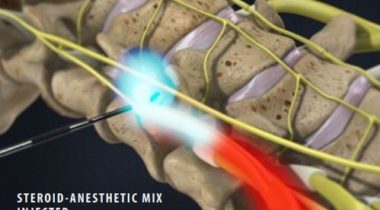
Transforaminal Epidural Injections
Transforaminal epidural injections are commonly performed to treat leg and/or back pain without surgery. This targeted approach delivers anti-inflammatory medication directly into the epidural space, where irritated nerve roots are causing pain. By reducing inflammation, the injection helps relieve pain and improve mobility.
How is this procedure done?
During the procedure, the patient is sedated but remains awake to help Dr. Reid monitor sensations. A small, blunt needle is inserted through the bony opening near the exiting nerve root, using fluoroscopic (live X-ray) guidance. This precise technique allows for more direct delivery of medication than traditional epidural approaches.
How effective are Transforaminal Epidural Injections?
Relief may begin within a few days and can last weeks to years depending on the individual. Often, patients receive a series of injections spaced over several weeks. Effectiveness varies, so it’s important to monitor your response and consult with Dr. Reid about further treatment options.
Caudal Epidural Injections
Caudal epidural injections deliver anti-inflammatory medication into the epidural space at the base of the spine, targeting inflamed nerve roots. This can help reduce lower back pain and symptoms that radiate into the legs. The injection is guided using fluoroscopy to ensure precise placement and effectiveness.
Who needs this procedure?
This treatment may benefit individuals suffering from conditions like spinal stenosis, sciatica, herniated discs, or radiculopathy. If your pain starts in the lower back and extends into the legs, Dr. Reid may recommend this procedure as part of your recovery plan.
How effective are Caudal Epidural Injections?
Many patients begin to experience relief within 3 to 5 days, with most noticing full improvement within 10 days. The duration of relief varies, and multiple injections may be scheduled for ongoing symptom management.
Cervical Epidural Injections
Cervical epidural injections are performed in the neck region to reduce inflammation and relieve pain caused by irritated or compressed nerve roots. This type of radicular pain may travel from the neck into the shoulders or arms. By injecting anti-inflammatory medication into the epidural space, swelling is reduced and the nerve roots are given a chance to heal.
Who needs this procedure?
Patients experiencing chronic neck pain, or pain radiating to the shoulders or arms, may benefit from cervical epidural injections. Dr. Reid can help determine if this treatment is appropriate during a detailed consultation and examination.
How effective are Cervical Epidural Injections?
Results vary depending on the cause and severity of the inflammation. Some patients experience pain relief lasting several weeks to months, while others may need a series of up to three injections spaced two weeks apart. In many cases, this treatment reduces the need for surgery or ongoing medication.
Horizontal Therapy
Horizontal therapy is an advanced electrotherapy technique administered at our office using the ProElec DT 2000. It simultaneously targets the bioelectrical and biochemical processes within the body, which are both critical for cellular communication. When communication between cells—whether in bone, muscle, ligament, or nerve tissue—is disrupted, pain and dysfunction occur. Unlike traditional treatments that address only one type of communication, horizontal therapy engages both, offering a comprehensive and effective pain management solution.
Who needs this procedure?
Horizontal therapy can help patients dealing with a wide variety of acute or chronic pain conditions, including:
- Migraine Pain
- Carpal Tunnel Pain
- Back Pain
- Tendonitis Pain
- Sciatica Pain
- Neck Pain
- Knee Pain
- Post-Op Pain
- Hand Pain
- Ankle Pain
- Arthritis Pain
- Wrist Pain
- Foot Pain
- Sprains
- Strains
- Shoulder Pain
×
Schedule an Appointment